抗加齢
Aging can be defined as any change to an individual over time. It is an inevitable process in human life. There is chronological aging and biological aging, although in general they go in parallel direction. As we age, we experience changes in our physical and psychological states.
There is a steady decline in the function of all body systems, such as the brain, heart, liver, and kidneys. It is associated with:
- Reduced protein synthesis
- Decrease in lean body mass and bone mass
- Increase in percentage of body fat
- Decrease in physical strength
- Decrease in memory and other cognitive functions
- Decrease in the ability to maintain a homeostasis and fight diseases
- Decrease in the overall quality of life.
Theories Of Aging
- Structures at the ends of chromosomes called telomeres have been shown to shorten with each successive cell division. This activates a mechanism that prevents further cell division, and provide a biological clock which will stop when the telomers are lost totally.
- Waste products and cross-linked compounds accumulate inside cells and interfere with metabolism.
- Increase in auto-antibodies that attack the body's tissues.
- Free-radicals, which are unstable and highly reactive organic molecule resulted from oxidation, cause damages to the body systems.
- The endocrine glands are depleted of their production, with a decrease in various hormones such as growth hormone and thyroid hormone.
Anti-aging
Anti-aging addresses how to prevent, slow, or reverse the effects of aging and help people live longer, healthier, happier lives. Many cultures developed long traditions of herbs, foods, diets, and health practices to foster anti-aging. The ultimate goals are to add life to years as well as to add years to life.
The nowadays anti-aging practices includes nutrition, physical fitness, skin care, aesthetic treatments, hormone replacements, vitamins and supplements. These target to give a youthful external appearance, and a strong healthy internal functions.
Bio-identical Hormone Replacement
Out of all the supplements administered into the body, hormones have been studied extensively, and there is much interest today in the use of anti-aging hormones. Many studies have shown a gradual decline in a number of hormones, and this decline may be responsible for some of the effects of the aging process.
Decline in oestrogen and progesterone in menopause for women, and their replacement, has been the subject of much research. Attention now appears to have focused on other hormones. These include:
- human growth hormone (HGH)
- the male hormone testosterone in men, and interestingly women
- the adrenal hormone dehydroepiandrosterone (DHEA)
- the pituitary hormone melatonin.
The decline in these hormones starts much earlier and is more gradual, as early as from 30 years old onwards. The relative deficiency of each of them leads to a variety of symptoms that may be reversed with their replacement.
We shall discuss the properties and applications of the individual hormones in the following sections.
更年期
Menopause means the cessation of a woman’s menstruation. Technically a woman has to have no menses for 12 months before she is described as menopausal.
During the reproductive years, oestrogens are produced from the ovaries, which stimulate the lining of the uterus for implantation of a fertilised egg, the beginning of pregnancy. The principle oestrogen of the menstrual cycle is estradiol.
As a woman enters her mid-thirties, her reproductive
capacity starts to decline, with a decrease of oestrogens
and progesterone production. During this time, however, she
usually continues to ovulate and her menstrual cycle generally
remains regular and normal.
When a woman reaches 40 - 45, her menstrual cycle can become
very disrupted and oestrogens levels can swing from very high
to very low. This can result in alternating sensations of
enlarged and tender breasts with bloating and irritability
when oestrogens are dominant; and hot flushes, confused thinking
or lack of concentration, memory difficulties and vaginal
dryness when the oestrogens levels plummet. There may be time
with no bleeding, followed by heavy bleeding accompanied by
severe cramps. This is referred to as peri-menopause, which
precedes the true menopause by 5 - 10 years.
Symptoms & Implications
At a woman enters the menopause, oestrogens levels have become so low that the lining of the uterus is not stimulated to build up enough to shed, and therefore periods no longer occur. These continued low levels cause:
- Increase in hot flushes
- Difficulty concentrating and memory problems
- Accelerated loss of bone at a faster rate than at any time in her life.
Other symptoms of the peri-menopause may intensify, such as:
- Vaginal dryness
- Decreased libido
- Dry skin
- Loss of skin elasticity
- Shrinking breasts
- Decreased mood and energy.
Few years after the menopause, the body will settle into a lower oestrogens state, and many women become acclimated to the symptoms. Bone loss slows down, but definitely continues. The damage to the many organ systems that need oestrogens continues insidiously, with increase in:
- Cardiovascular disease
- Osteoporosis and fracture
- Diabetes
- High blood pressure
- Strokes
- Alzheimer's disease.
The aging of a woman's reproductive system is actually a fairly continuous process that starts in the early thirties. An anti-aging approach takes this into account, and intervenes before the actual menopause to treat the symptoms and long-term consequences that result from less than optimal hormone levels.
Diagnosis
Apart from the clinical symptoms and signs that accompany the cessation of menstrual periods, blood tests can be done to measure the levels of estradiol and progesterone.
Treatments & Options
This is done through Hormones Replacement Therapy, which include estradiol, progesterone, and in cases, the male hormone testosterone too. This is discussed in the sections of Oestrogens & Progesterone, and Testosterone.
男性更年期
Every healthy male will have a decrease in the production of androgens - the male hormone, as he ages. The principle androgen in focus is testosterone. When the serum testosterone levels in an older man decline to below the normal range in young men, and that person experiences clinical symptoms and signs consistent with androgens deficiency, then andropause has occurred.
This decline in testosterone is gradual, spanning ten to fifteen years on average. This gradual decrease of testosterone does not display the profound effects compared to the menopause in women, particularly there is no such abrupt cessation of something like the menstruation. The onset of symptoms is gradual and vague, and can be easily missed. However, at the end, the consequences on health are similar.
30 - 40 is the age when testosterone levels begin to start their age-related decline. In fact, by their 50s, 50% of men have a significant reduction in bio-available testosterone.
Symptoms Of Andropause
Depression
Androgen deficiency can affect cognitive functions, resulting
in lack of mental energy, decreased sense of well-being and
depression.
Fatigue
Androgen deficiency causes loss of lean muscle mass, tone
and bone density. These losses can leave an andropausal man
with feelings of fatigue. There is also a multitude of generalised
aches and pains throughout their bodies.
Irritability
Androgen deficiency can also heighten feelings of irritability
that can lead to aggression, hostility, and anger.
Reduced Libido & Sexual Performance
Androgen deficiency reduces libido and causes erectile dysfunctions,
which include difficulty in achieving an erection, the time
of an erection, diminished force and volume of ejaculation,
diminished rigidity of the erection and diminished pleasure.
Sweating & Flushing
As with women, the fluctuating levels of hormones can cause
periods of diffuse sweating and hot flashes.
Diagnosis
Andropause is often under-diagnosed because symptoms can be vague and vary among individuals. Some men even find it difficult to admit that there is a problem, and doctors may consider the symptoms being related to other medical conditions, such as depression, diabetes, or simply aging which is an inevitable thing that nothing can or should be done.
This situation has changed dramatically and more doctors are actively diagnosing and treating andropause. A screening test called the ADAM (Androgen Deficiency in Aging Men) test and a laboratory measurement of testosterone can be done.
ADAM Test
The ADAM test is a questionnaire used to screen for symptoms of low testosterone in men over 40.
- Have you experienced a decrease in your sex drive (libido)?
- Do you lack energy?
- Have you lost height?
- Has your strength and/or endurance decreased?
- Have you noticed yourself enjoying life less?
- Are you frequently sad or irritable?
- Are your erections less strong?
- Have you noticed a recent deterioration in your athletic ability?
- Do you find yourself falling asleep after dinner?
- Has there been a recent deterioration in your work performance?
Bio-Testosterone Test
If your ADAM test seems to suggest andropause, the best test to follow is to determine low testosterone levels with the Bio-T Test.
The Bio-T Test measures levels of "bio-available testosterone", which is the testosterone not bound to the carriage-protein, Sex Binding Hormone Globulin (SHBG), and is freely available for the body to use on demand.
Treatment
This is achieved through Testosterone Replacement Therapy (TRT), which has been shown to be a very safe and effective treatment for men who have been diagnosed with andropause. The details are discussed in the section of testosterone.
ヒト成長ホルモン (Growth Hormone)
Human Growth Hormone (HGH), also called somatotrophin, is produced in the anterior pituitary gland by the somatotroph cells. HGH is secreted in short pulses lasting 1 - 2 hours, predominantly at night during deep sleep. HGH secretion is controlled by the hypothalamus through a negative feedback mechanism by the effects of other hormones. Exercise is proven to stimulate the release of HGH.
As HGH circulates through the blood, it stimulates the production of insulin-like growth factor I (IGF-I), mainly by the liver. In addition to the role in promoting linear growth in children, it is also an anabolic hormone with stimulatory effects on protein synthesis, and the break down of fat.
HGH was used to treat dwarfism or short-stature in children, and in cases of absolute growth hormone deficiency in adults, where the pituitary gland cannot produce HGH because of other problems.
HGH used to be made from human cadaver pituitary glands, which was expensive, and had the risk of contracting a brain disease similar to the mad cow disease. Now it is made from a recombinant DNA technology (gene cloning), which enables a production of large quantities of pure, uncontaminated human growth hormone.
Measurement of HGH
Because HGH is released in spurts, a single measurement is of no value in assessing the 24 hours secretion. The blood level of IGF-I, in contrast, is more constant, and therefore it serves as an indirect but reliable measure of HGH activity.
From the third decade, an increasing proportion of men and women show decreases in growth hormone secretion and serum levels of IGF-I from the peak. Analysis has estimated an approximate 14% reduction in HGH production for each decade in adults, and it is believed that reduced HGH secretion and IGF-I account, at least in part, for the effects of aging.
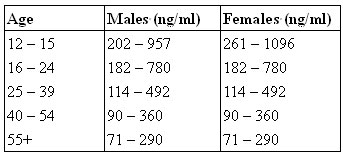
Reference ranges of IGF-I for different age group:
Human Growth Hormone & Aging
In adults where there is a true and absolute deficiency of HGH, they appear to be suffering from premature aging, with twice the rate of death from cardiovascular disease compared with age-matched controls; increased abdominal fat; decreased muscle mass and strength; increased fatigue, social isolation and depression; and poor performance at work.
When these people are treated with the recombinant HGH, virtually all of these aspects of premature aging were reversed with one year of treatment, but they return to baseline when the therapy is stopped.
In ordinary adults, researches had shown that HGH replacement in men, when restoring the IGF-I level to the youthful range, can reverse the well-known body composition changes associated with aging, such as decreased muscle tone, increased abdominal fat, and thinning skin. With six months of therapy, there is on average 8.8% increase in lean body mass; 14% decrease in fat mass, predominately around the waist; 7% increase in skin thickness; 1.4% increase in bone density; and a greater sense of well-being. It is said that these changes are equivalent in magnitude to the changes incurred during 10 to 20 years of aging.
Growth Hormone Replacement Therapy
With the latest recombinant DNA technology, unlimited amount of HGH can be manufactured. The production uses mammalian cell lines and are identical structurally, chemically, and biologically to natural HGH. There is no risk of bacterial protein contamination, and allergic reactions from the immune system.
The HGH is administered by injections into the deep subcutaneous tissue or into the muscles. Today manufacturers have prepared injection pens, which the patients can use at home. They are easy to use and can be adjusted to deliver the exact number of HGH units required.
The amount of HGH prescribed, and the benefits achieved, depend on your starting level of IGF-I. If your level is below 100 ng/ml, you will likely see significant changes in body composition in the first six months. If you have a higher level, the effect of the supplementation may be to prevent these age-related changes from occurring.
Potential Benefits
- Decrease in fat mass, after approximately 6 months, predominantly around the waist, without change in diet and exercise.
- Increase in lean muscle mass, after six months.
- Increase in skin thickness, and hydration of the skin.
- Improved bone density after one year of therapy, depending on pre-treatment density.
- Improved cardiac and lung functions, lowered diastolic blood pressure.
- Decreased total and LDL cholesterol levels, and increased HDL levels.
- Accelerated wound healing.
- Increased immune system functioning.
- Increased physical and mental energy levels.
- Improved sleep, vision, and mood.
Side Effects & Safety
There is ample evidence to support the safety of growth hormone replacement therapy in growth hormone deficient adults, and it is likely that the same safety profile pertains in aging adults.
Side effects have been reported but were mainly related to HGH being given in much higher doses than necessary to get the body composition changes expected.
Side effects are mainly related to fluid
and sodium retention, which consist of oedema, joint and muscle
pain, and carpal tunnel syndrome (nerve trapped by the swelling
in the wrists). These problems resolve when treatment is stopped.
Similar side effects are reported in patients on lower doses,
if growth hormone is started when the patients are over 65
years of age. A low level of side effects is observed when
HGH is started in men between the ages of 48 and 66, while
losing more body fat and gaining more lean muscle. This is
probably because the majority of the decline in growth hormone
secretion takes place before age 50, and therefore it should
start to be replaced at a younger age, before the body has
been with a very low level of GH for decades.
Therefore, when HGH replacement is started in younger patients,
there are very few side effects. When started in older patients,
it must be started at low doses and increased very gradually.
Growth Hormone Secretogogues? BEWARE!
There are a lot of oral preparations available in the market, and they all claim to be either pure HGH, or effective in stimulating the release of HGH in blood, with absolutely no side effects whatsoever. The benefits listed are many and extremely persuasive with comments from previous users, sometimes celebrities, in the forms of well-written testimonials. Information on their composition and pharmacology is very sketchy and is often not provided. It is a serious question what these products really are.
There is no clinical evidence that any food or herbal supplement can achieve the benefits of the real HGH replacement therapy. There are some oral forms of Growth Hormone Releasing Hormone or its related peptides, which can indeed cause more release of HGH. However, the clinical use of these products are not well studied yet, and would equally have the same side effects profile as HGH, and so cannot be 100% safe to buy and take as the patients wish under no supervision.
テストステロン (Testosterone)
Testosterone is the main male hormone. 95% of it is produced in the testicles, under the influence of Luteinising Hormone (LH), which is released in spurts throughout the day from the pituitary gland. The signals are stronger in the early morning, which accounts for the higher testosterone levels and the spontaneous morning erections and increased libido. By late evening the levels can fall by 50 percent.
About 97% of testosterone in the blood is bound to a protein called Sex Hormone Binding Globulin (SHBG). These are not freely available, and serve as storage to maintain a steady supply for the tissues. Only the free testosterone is biologically active.
In addition to the testicular production, a smaller amount is created by the conversion of precursor steroid hormones such as androstenedione and androstenediol. However, if supplemented, androstenedione gets converted into more oestrogens than testosterone, and therefore there is not a sustained muscle enhancing effect, but often results in feminisation of the user.
Measurement of Testosterone
The Bio-T Test measures levels of bio-available testosterone, which is the portion either unbound, or bound to albumin, but not bound to SHBG.
The normal range reported on a laboratory report runs from about 290 to 900 ng/dl. However, it is the range for the whole population, covering men of all age groups and health statuses. They can be 80 or 20 years old; they can be chronically ill or very healthy; and they can be obese or thin. It is therefore not for any particular individual of a specific age. Unfortunately, most doctors think that if the test value falls in this range, then there is no problem.
Testosterone & Aging
Like the growth hormone, testosterone levels decline with age in healthy males. Total testosterone levels declined by about 5% per decade from the 30s to the 70s. Bio-available testosterone declines twice as fast, about 10% per decade, so that approximately 50% of men over 55 years old have levels below the lowest normal range for young men.
When testosterone drops to an absolute low level below 300 ng/dl, it is called hypogonadism. Virtually all men below this range exhibit the signs and symptoms. Relative deficiency in a man with symptoms and signs may be regarded as the andropause. Typical responses to low bio-available testosterone levels include:
- Low sex drive and sexual performance
- Emotional, psychological and behavioural changes
- Decreased muscle mass
- Loss of muscle strength
- Increased upper and central body fat
- Loss of height
- Bone loss
- Decreased energy
- Frequent fatigue
- Low red cell counts (anaemia)
Testosterone Replacement Therapy (TRT)
There is extensive evidence that replacing testosterone in hypogonadism is warranted, and there is no controversy that it should be treated. However, when the serum testosterone levels in a middle age or older man decline to a level above 300 ng/dl, but below the normal range in young men, and that person experiences clinical symptoms and signs consistent with androgen deficiency, he can benefit from a boost with TRT to the high end of normal or even above that. This is the use in andropause.
A number of studies have been done in healthy young men in whom doses of testosterone were given that raised their levels into the high adolescent range of 1000 to 2000 ng/dl. In all of these studies, lean muscle mass has increased and fat mass has decreased. Similar studies with lower doses have been done in moderately obese men; again, lean mass increased and fat decreased even more. Moreover, insulin resistance improved, triglycerides decreased, and energy increased. Many more studies have been published showing similar effects in older men over 65 with mildly low testosterone levels. The accumulating evidence shows that whenever you raise the testosterone level, no matter what the starting level, you get benefits in body composition, without any significant increase in adverse effects.
Once started, the medication should begin to reverse the signs and symptoms of andropause relatively quickly. However, just as andropause tends to have a slow and subtle onset, the reversal will also be slow and subtle, so it is important to stick with it for at least 3 months, and keep track of how the symptoms change. There is also the possibility that your starting dose may need to be increased.
Some problems may get better faster than others. You may notice improvement in your mood, thinking and concentration within a few short weeks, while other changes may take a little longer.
Treatment Options
There are a number of types of testosterone replacement treatments available. These include: pills to take by mouth, transdermal patches and gels applied to the skin, and injections. There are pros and cons to each method and you should discuss these choices with your doctor.
Alternatively, Human Chorionic Gonadotropin (HCG), which is a hormone that stimulates the testes to produce testosterone on their own, can be used. Only injection is available.
Potential Benefits of TRT
Basically the symptoms are reversed. They include:
- Improvement in mood and sense of well-being
- Increased mental and physical energy
- Decreased anger, irritability, sadness, tiredness, nervousness
- Improved quality of sleep
- Improved libido and sexual performance
- Potentially less bone degradation and an increase in bone density
- An increase in lean body mass,
- Decreased body fat, particularly around the waist
- Increased muscle strength
Side Effects & Safety
Prolonged erection is a possible complication of testosterone replacement treatment. Occasional, if used at high doses, testosterone may be converted to oestrogens, and leads to enlarged breasts.
There is no evidence that testosterone may increase the risk of benign prostate enlargement, or prostate cancer. Nevertheless, it is recommended that elderly patients on testosterone treatment should have the prostate examined annually, together with ultrasound, and a blood test for prostate-specific-antigen (an indicator for prostate cancer) every 6 months.
There is conflicting evidence whether testosterone has more beneficial or adverse effects on the cardiovascular system.
Other concerns include its effects on sleep apnoea, hair growth and baldness, as well as too high a blood count.
In general, men with known prostate cancer, significantly enlarged prostates, or breast cancer should not receive TRT. There is also some question as to whether it should be used in men with sleep apnea.
Testosterone & Women
Just as for men, testosterone is important for maintaining lean muscle mass, assertiveness, and bone density in women. It is also important for warding off depression, increasing libido, and maintaining the health and sensitivity of the vaginal tissues. The difference is that women only need about a tenth of the circulating testosterone as men do.
Approximately 30% of a woman's testosterone is produced in the ovaries; the other 70 % is derived from conversion of adrenal androgen precursors, such as DHEA and androstenedione, both of which decline with age. So a woman will have a decline in her testosterone level as she ages. This is a gradual decline, and on average, there is a 50% drop in testosterone level between age 20 and 50, before menopause occurs.
When the ovaries are removed for other medical reasons, there is an abrupt drop in her testosterone production. The women may feel unwell, with drop in libido and weight gain, even when they are on adequate oestrogens replacement. Also, post-menopausal women may continue to lose their bone mass even on apparent adequate oestrogens replacement, but the bone density may be normalised when testosterone is added.
The free testosterone level can be measured and is probably on the low side. In the peri-menopausal period and after the menopause, in a woman with intact ovaries, restoring DHEA to youthful levels will often restore the testosterone levels adequately. In a woman who has had her ovaries surgically removed, it is usually necessary to start directly with bio-identical testosterone replacement. This is usually prescribed as a cream to be applied to the skin.
甲状腺ホルモン
The thyroid is a small gland located in the front of the throat. It secretes thyroid hormones T3, which is converted to T4 in the blood. The secretion is stimulated by Thyroid Stimulating Hormone (TSH) from the anterior pituitary gland. Thyroid hormone affects all the metabolic processes, from body temperature to heart beat. The activity of the thyroid gland can be assessed by measuring the levels of TSH, free T3, and free T4.
Hashimoto’s disease, the most common cause of low thyroid levels, is an autoimmune disorder in which the immune system attacks the thyroid gland making it unable to produce adequate levels of thyroid hormones.
Features of Hypothyroidism
- Increased susceptibility to infection
- Muscles cramps
- Persistent low back pain
- Easy bruising
- Mental sluggishness
- Emotional instability
- Feel cold easily
- Dry, coarse and pale skin
- Coarse and sparse hair
- Anaemia
Thyroid Hormone & Aging
The incidence of frank hypothyroidism is much higher in the older age group. However, thyroid hormone does not have the age-related decline characteristic of HGH or DHEA. Its deficiency is common in the population, with 15 - 40% of people suffering in some way from a relatively under-active thyroid.
Apart from the features mentioned above, thyroid deficiency can be translated into risk of age-associated diseases:
- Increased risk of adult-onset diabetes
- Increased levels of cholesterol and triglycerides
- Increased risk of heart disease and high blood pressure
- Dementia and other impaired cognitive functions, such as slow thinking, difficulty in concentration, and poor memory.
Thyroid hormone replacement therapy is one of the unabashed successes of modern clinical medicine. It is a standard practice to replace the thyroid hormone when a patient has the above features of hypothyroidism and a low T3 and T4 measurement.
Side Effects & Safety
It should be done under medical supervision, with regular blood tests to check for appropriate levels of TSH, free T3 and free T4. Too much replacement will result in potentially dangerous side effects, such as excessive bone loss, high blood pressure, and abnormal heart rhythm.
メラトニン
Melatonin is produced by the pineal gland, a small organ set behind and between the eyes. This gland receives direct input from the eyes so that it knows when it is daytime and nighttime. Melatonin is released in spurts at night to initiate sleep, and wanes upon daybreak, when bright light signals the production to shut down.
Because of this, taking melatonin at bedtime can be effective in resetting the clock of a person who changes time zones, thereby alleviating “jet lag.”
Melatonin & Aging
Melatonin levels are highest in children, and less and less melatonin is produced as we age. By age 60, we produce less than 50 % of the melatonin as we did at 20.
Pineal gland transplanted from old mice to young mice was found to speed up the aging, whereas the reverse made the old mice regain youthful functions. Melatonin supplementation also extended the life span of mice by 25%.
Thymus gland is a key organ of the immune system involved in the production of T-cells to fight diseases. It is largest when the melatonin levels are highest around puberty, and shrinks as the melatonin levels decline. Melatonin supplementation in mice was found to increases the weight of the thymus gland again.
Melatonin Replacement
It is recommended that patients take melatonin regularly at bedtime starting at age 50 and increasing the doses as they get older. To find the dose that works for you, start with the lowest amount, about 0.5 to 1mg, 1 to 2 hours before bedtime. Decrease the amount if you feel drowsy in the morning, or increase it if you have trouble sleeping.
There are two types of melatonin that may be used in these pills: natural and synthetic. Natural melatonin is made from the pineal gland of animals. This form could be contaminated with a virus and is therefore not recommended. The synthetic form of melatonin does not carry this risk.
Potential Benefits
Melatonin is a strong anti-oxidant that removes the harmful free radicals from the body. Free radicals are major contributors to aging and the diseases of old age – heart disease, cancer and autoimmune disorders.
Melatonin also boosts the immune system, particularly those aspects that fight cancers.
A common problem with aging is difficulty sleeping. Melatonin reduces the time to fall asleep, increases actual sleeping time, reduces the number of awakenings, and increases the quality of sleep. Better and deeper sleep in turn promotes more secretion of human growth hormone.
デヒドロエピアンドロステロン (DHEA)
DHEA has been dubbed the “mother of all steroids”. It is the most abundant steroid in the body and is involved in the manufacture of testosterone, oestrogens, progesterone, and corticosteroid. It is in the sulphated form (DHEAS) when circulating in the blood.
DHEA & Aging
Its blood level declines continuously and sharply from adolescence to old age, and parallels to that of HGH. By age 65, the production drops to about 10 - 20% of that at age 20.
Its decline has been correlated with an increased risk of death from cardiovascular disease in men (not women), decreased immune system function in both sexes, decreased insulin sensitivity, and decreased IGF-I levels.
Out of a group of men between 60 and 80, those with the highest levels of DHEA were younger, leaner, and more fit and had higher testosterone levels than those with the lowest levels.
DHEA Replacement Therapy
DHEA is just one of the important hormones in an overall hormone replacement therapy program. It may mediate some of its anti-aging effects through increasing the levels of IGF-I, although it does not affect the HGH level itself.
It is readily available in health food store. Dosages commonly range from 25 to 150mg, but it is best to start at the lower end at 25 - 50mg per day, and raise the dosage later if necessary. 50mg is usually all that required to bring DHEA up to youthful levels.
Although there is no evidence that its use causes an increased risk of breast or prostate cancer, but if one already has either of these cancers it can cause increased growth of the tumour because the body can convert it into estradiol and testosterone. Therefore it is recommended to screen for breast cancer with a mammogram and a breast exam; and prostate cancer with a PSA and rectal exam prior to starting therapy.
Potential Benefits
- Increase in lean muscle mass
- Decrease in fat mass
- Increase in immunity function for killing viruses and tumor cells
- Reduce risk of age-related diseases, including cancer, heart disease, and osteoporosis
- Improve blood sugar control and prevent diabetes
- Improve auto-immune diseases such as lupus
- Increase responses to vaccines
- Protect against Alzheimer’s disease
- Increase in perception of psychological and physical well-being
- Better sleep, increased energy, less stress
- Increase life expectancy
エストロゲンと プロゲステロン
Oestrogens
Oestrogens refer to a class of molecules that have oestrogen-like activity in the body. Many molecules are oestrogens, but the principal oestrogens in a woman are estradiol, estrone, and estriol, but each with a different degree of effectiveness in different tissues.
Estradiol is the most potent of the oestrogens produced by the ovary. A very small amount circulating in the blood can cause potent changes in oestrogen-responsive tissues. Estrone is a metabolite of estradiol and is considerably less potent. Estriol is a further metabolite of estradiol and is quite weak.
Estradiol, estrone, estriol, and all of their metabolites are bio-identical hormones found naturally in the body. Bio-identical hormones are defined as compounds that have exactly the same chemical and molecular structure as hormones that are produced in the human body.
In contrast, the most commonly prescribed oestrogens formulation for hormone replacement therapy is a mixture of estradiol, estrone, and 10 or more horse oestrogens that are exogenous to humans. Some of these hormones are very potent oestrogens, even more so than estradiol. Unfortunately, there are no readily available tests for monitoring the levels of these foreign hormones.
Menopause & Aging
The decline of oestrogens and progesterone is not gradual like other hormones.
As a woman enters her mid-thirties, her reproductive capacity starts to decline, with a decrease of oestrogens and progesterone production.
When she reaches 40 - 45, the oestrogens levels can swing from very high to very low. This can result in alternating sensations of enlarged and tender breasts with bloating and irritability when oestrogens are dominant; and hot flushes, confused thinking or lack of concentration, memory difficulties and vaginal dryness when the oestrogens level plummets. There may be time with no bleeding, followed by heavy bleeding accompanied by severe cramps. This is referred to as peri-menopause.
5 - 10 years later the menopause finally arrives, the production of oestrogens and progesterone by the ovaries stops completely and results in permanently low levels, which can be measured by blood tests. Replacement of oestrogens and progesterone is a common and effective treatment for symptoms associated with menopause.
Potential Benefits of Replacement
The low oestrogens levels can cause a lot of undesirable effects on the body:
- Hot flushes
- Vaginal dryness
- Decreased libido
- Dry skin & loss of skin elasticity
- Shrinking breasts
- Decreased mood and energy
- Difficulty concentrating and memory problems
- Cardiovascular diseases
- Accelerated bone losses
- Osteoporosis and fracture
- Diabetes
- High blood pressure
- Strokes
- Alzheimer's disease.
Hormone replacement therapy (HRT), particularly with the bio-identical hormones, may reverse many of these problems and risks.
Treatment Options
Oral
- The majority of women take their HRT in pill form by mouth. While very convenient, a large amount of oestrogens goes through the intestines and then hits the liver within a short period, which is different from the gradual release of oestrogens from the ovaries. This changes the metabolism of the liver and results in a number of deleterious effects:
Increase in clotting factors, hence the possible side effect of causing an increase in blood clots in the leg veins. - Increase in sex hormone binding globulin (SHBG), which binds more testosterone and results in symptoms of low testosterone - decreased libido, vaginal dryness, thinner bones, loss of lean muscle and increase in fat.
- Alcohol intake will dramatically increase the level of oestrogens to as much as 300%, which is even higher than in a normal menstrual cycle. This may be one of the causes of an increased risk of breast cancer with oral HRT.
- Increase in the incidence of gall stones.
- Increase in triglycerides, which is a risk factor for heart disease.
- Increase in C-reactive protein, which is a potent risk factor for coronary artery disease.
Transdermal
With transdermal application, the daily dose is released gradually into the circulation, just as when the ovaries are functioning naturally. As a result, the above problems occur much less likely, and there is only a 30% increase in oestrogens level with alcohol consumption.
This can be done by either a patch, or transdermal cream.
Side Effects & Safety
The most commonly reported adverse events of oestrogens include headache, breast pain, irregular vaginal bleeding or spotting, stomach or abdominal cramps, bloating, nausea and vomiting, and hair loss.
There is some controversy regarding the positive or negative effect of HRT in causing cardiovascular diseases and breast cancer. There seems to be an increased risk when taking oral HRT. Doctors supporting the opposite say that bio-identical HRT taken transdermally is safer, more effective and does not have the same problems.
A menopausal or post-menopausal woman should discuss her individual risks and benefits of HRT with her doctor. If she decides that HRT would be overall beneficial, then she should go ahead with a regime but with close monitoring as well.
In general, the following advices are still being made:
- It increases the chances of cancer of the uterus
- It may increase the chance of heart attacks, strokes, breast cancer and blood clots.
- It should not be used if you have unusual vaginal bleeding, currently or have had blood clots, certain cancers, had a stroke or heart attack in the past.
It may be popular to get the HRT from some compounding companies who make the custom-mixed formula, but they may pose risks in terms of purity, potency, efficacy, or safety. Bio-identical estridiol and progesterone are available in approved hormone replacement products, which come in many different doses and forms (patch, cream and gel).
Progesterone
Progesterone is secreted by the corpus luteum, which is the residual body after the ovulation. It serves to counteract the continuous stimulation on the uterine lining by oestrogens, and causes the regression of the lining, to result in a menstrual period, if the egg has not been fertilised.
It is prescribed together with oestrogens in HRT because it can protect the uterine lining from over stimulation, and therefore reduce the risk of cancer in the uterus.
One of the most commonly prescribed preparations is medroxyprogesterone acetate, which is formed by the addition of a molecule to progesterone, so that it is patentable and more orally absorbable. However, women who take this often feel irritable, depressed, have mood swings, fluid retention and bloating. On the contrary, bio-identical progesterone elevates mood and is calming, and there is complete resolution of the adverse symptoms when women are switched away from
medroxyprogesterone acetate.
In addition, bio-identical progesterone was found to have the best effect on HDL cholesterol, and does not have the potential negative effect in increasing the risk of coronary artery diseases. This may explain the results of some trials, which showed that oestrogens do not protect the heart as was thought, when it is combined with medroxyprogesterone acetate. The early slight increase in heart attacks in women with established cardiovascular disease could have resulted from its negative effect on the coronary arteries.
Replacement therapy can be delivered transdermally as patch or cream, which is better than taken orally in capsules.