Hair Structure & Growth
Humans have around 100,000 to 150,000 hairs on the scalp. Adult Asians have around 100,000, while adult Caucasians have around 150,000. The actual number depends on the amount of hair follicles, and the density of hair follicles will decrease as we age. During childhood, the density is around 1000 / cm2, reducing to around 600/cm2 in young adulthood, and 300/cm2 or less in later life.
Hair Types
The hair follicles are formed as early as the 9th to 12th week in the fetus, and are widely present from the 4th month onwards. There are three types of hair: the Lanugo Hair in the fetus and baby; the mature fine Vellus Hair; and the mature robust Terminal Hair.
The lanugo hairs are extremely fine and soft, covering the whole fetus. They are mostly lost before birth, although occasionally some may persist in the first month of the newborn babies.
Vellus hairs usually have a length no longer than 1 - 2 cm. They are fine, have a lighter colour, and are present all over the body. They are not connected with the sebaceous (oily) glands, and therefore do not have oily secretion. The “mustaches” in females consist of vellus hair, whereas those in the males are terminal hair.
Terminal hairs are regional and do not cover the whole body. They are those on the scalp, the mustaches in males, the underarm hairs, the pubic hairs, and the hairs on the limbs. They have a growth cycle, and are connected to sebaceous glands, with oily secretion coming out from the hair follicles to lubricate the skin.
The Hair Growth Cycle
The hair shafts are made from the hair follicles. The growth starts from budding, to getting strong, thick, and increase in length, and finally shed off. The cycle can be divided into three phases: growth phase (Anagen); degradation phase (Catagen); and resting phase (Telogen).Anagen The hair bulb and the follicle are closely adhered. The follicle continuously produces new hair shaft. The hair growth will last for 2 to 4 years and the average rate is about 1 cm per month. The longer the anagen phase, the longer the hair will be. This depends on the race, the sex, and the age. Females of course have a longer anagen phase. As we age, the anagen phase will get shorter.
Catagen The bulb and the follicle gradually separate. The bulb will form a round end and the follicle begins to stop its production of hair shaft. The hair growth is slowed down and the hair begins to degrade. This phase lasts for about 2 - 4 weeks.
Telogen The hair follicles shrink, and the hair growth come to a complete stop. This resting phase lasts for 2 - 4 months. Shedding of the hair occurs only after the next growth cycle (anagen) begins and a new hair shaft begins to emerge.
Under normal circumstances, 90 - 95% of hair is in growth phase, 5 - 10% in resting phase, and less than 1 % in degradation.
On average 50 - 100 telogen hairs are shed every day. This is normal hair loss and accounts for the hair loss seen every day in the shower and with hair combing. These hairs will regrow. A variety of factors can affect the hair growth cycle and cause temporary or permanent hair loss (alopecia) including medication, radiation, chemotherapy, exposure to chemicals, hormonal and nutritional factors, thyroid disease, generalized or local skin disease, and stress.
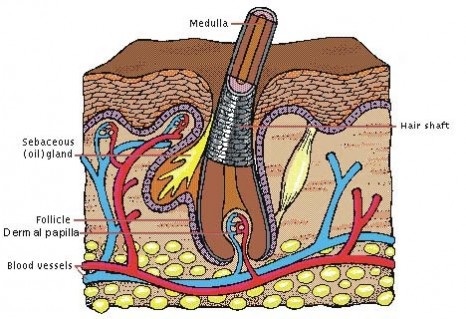
The Hair Structure
Hair is composed of strong structural protein called keratin. This is the same kind of protein that makes up the nails and the outer layer of skin.The hair consists of the hair shaft and the hair bulb. The bulb is closely adhered to the follicle and receives nutrients through blood supply. The stem cells in the bulb split into different cells, which are arranged concentrically as they move up the hair. After many processes of compression and hardening, these cells become dead keratin and form the tough hair shaft.
|
|
Each strand of hair shaft consists of three layers.
- An innermost layer called the medulla, which is basically empty, and only present in large thick hairs.
- The middle layer is known as the cortex, which provides strength, and both the colour and the texture.
- The outermost layer is known as the cuticle, which is thin and colorless. There are 6 - 10 layers, overlapping like the tiles on the roof, and serves as a protector of the cortex.
Below the surface of the skin is the hair root, which is enclosed within a hair follicle. At the base of the hair follicle is the dermal papilla. The dermal papilla is feed by the bloodstream which carries nourishment to produce new hair. The dermal papilla is a structure very important to hairgrowth because it contains receptors for male hormones and androgens, which regulate hair growth.
Causes of Hair Loss
Hair shedding is actually a very normal situation of simple metabolism. The amount of hair loss is related to the growth phases. Under normal circumstances, 90 - 95% of hair is in growth phase, 5 - 10% in resting phase, and less than 1% in degradation. Any factors that interfere with these phases will alter the cycles. If the amount of hair in the growth phase is decreased, while those in the degradation and resting phases is increased, then more hair will be lost.
On average 50 - 100 telogen hairs are shed every day. This is normal hair loss and accounts for the hair loss seen every day in the shower and with hair combing. These hairs will re-grow. A variety of factors can affect the hair growth cycle and cause temporary or permanent hair loss (alopecia) including medication, radiation, chemotherapy, exposure to chemicals, hormonal and nutritional factors, thyroid disease, generalized or local skin disease, and stress.
Only when the number of hair shed each day is far more than 100, then hair thinning or balding will occur.
Hair loss can be divided into Generalised and Localised causes.
Generalised Hair Loss
- Androgenic Alopecia
- Telogen Effluvium
- Drugs
- Thyroid Diseases
- Iron deficiency
Androgenic Alopecia
This is the most frequently encountered situation and will be discussed in the next section.
Telogen Effluvium
This is because all the hairs suddenly enter into the degradation phase, and then all are shed. This usually happens in cases of acute severe illness, or the first 3 months after pregnancy. Other causes include major surgery, or extreme fasting such as anorexia. This causes a great alarming concern, but is only temporary, and will return to normal after a certain time. No treatment is necessary.
Drugs
Many drugs can lead the hairs into the degradation phase, and subsequent falling. This usually happens in a few weeks after starting the drugs, and returns to normal in a few months after stopping them.
|
Examples: |
|
|
Blood thinning drugs |
Heparin |
|
Warfarin |
|
|
Psychiatric drugs |
Amitriptyline |
|
Lithium |
|
|
Haloperidol |
|
|
Anti-epileptics drugs |
Carbamazepin |
|
Anti-inflammatory drugs |
Indomethacin |
|
Anti-thyroid drugs |
Carbimazole |
|
High blood pressure drugs |
B-blockers |
|
Vitamin A derivatives |
Retinoids |
|
Anti-parkinson drugs |
L-Dopa |
|
Bromocriptine |
Majority of these medications are prescribed because they are necessary, and therefore it may not be possible to discontinue them. If they are suspected to be causing the hair loss, do not just stop them, but seek the doctor’s advice.
It is commonly known that chemotherapy for treating cancers will cause total hair loss. This is because the chemotherapy will target any high-growing cells, including the continually splitting cells in the hair bulb. The hair will grow back after the chemotherapy is stopped.
Others
Throid problems, either over or under activity, chronic liver diseases, and iron deficiency can all cause a generalised hair loss. When the problems are corrected, the hair loss will slowly return to normal too.
Localised Hair Loss
- Alopecia Areata
- Trichotillomania
- Traction Alopecia
- Tinea Capitis
Alopecia Areata
Please go to the following sections.
Trichotillomania
This is due to uncontrolled and un-aware repeated pulling and twisting of the hair, causing the hair to be broken at different lengths, but not to the stage of balding.
It usually happens in children and adolescents, because of some psychological upset. The sufferers will deny this behaviour. What needs treatment is their psychology.
Traction Alopecia
This is due to unsuitable method of hair styling, for example when the hair is pulled back too tightly into a ponytail over along period of time will cause hair loss in the front hair margin.
Tinea Capitis
Please go to the following sections.
Androgenic Alopecia
Male baldness is an extremely common problem affecting hundreds of thousand of males. Some males are having baldness as early as in their 20’s. The incidence increases as they get older, around 40% of males in their 40’s and around 50% in their 50’s. Hair lost may be permanent.
According to a research, 77 % affected males think it makes them look older, 48% think it makes them look unattractive, 25% think it lowers their overall confidence, and 13% think they job prospect is worse because of this.
Cause of Male Baldness
There is a heavy genetic component, either from the father’s or the mother’s side. The level of a male hormone called Dihydro-testosterone (DHT) in the scalp has increased many folds, or that the hair follicles are more sensitive to a normal level of DHT. DHT will decrease the growth phase of the hair growth cycle, and the amount of hair lost per day will be more than normal.
Signs
The hair will gradually become thinner and sparse. Firstly it is the angle of the forehead being affected. The hairline recedes when more hair has fallen off, and later the hairline becomes M-shaped. Then the hair in the centre of the scalp follows, and slowly it becomes bald. At the last stage, the front and the centre merge together, leaving only the hair at the sides and the back of the scalp.
|
|
|
|
M-Shaped Forehead |
Central Baldness |
However, some people have the hair loss starting in the centre first, without losing hair at the forehead corners. When Androgenic Alopecia happens in the females, they will only have thinning in the centre too through out the whole process. In males, the degree of hair loss is staged using the Hamilton-Norwood Grades, while that in the females is staged using the Ludwig Classification.
Hamilton-Norwood Grades 1 to 8

Ludwig Classification Stages 1 to 3
Alopecia Areata
Alopecia areata is commonly seen in children and young adults. 10 to 20% has a family history.
Cause
This is related to a disorder of the immune system, which somehow does not recognise the hair follicles as self and attack them as if they are foreign. Among the sufferers, many have other auto-immune problems as well. 4 % of them has vitiligo, and up to 25% of children have abnormal thyroid functions or antibody against the thyroid.
Signs
The area of hair loss is not itchy or tender. There is usually no feeling. The person suffering from it may notice this only when they touch a smooth round patch of skin on the scalp by chance, or when they are told the presence of this by the hairdresser.
There are one or more round areas, which are smooth and not inflamed. The sizes may range from less than 1 cm to more than 10 cm across. At the margins, the hair may appear thinner at the bottom end and looks like an inverted exclamation mark.

When new hair grows back in that area, they are fine, fragile, lack of lustre, and may appear white. They are slowly replaced with normal hair. There is no scar after recovery.
Although alopecia areata affects mainly the scalp hair, but 10% can happen outside the scalp, such as the eyebrows, eyelashes, and mustaches. Few people may progress to the whole scalp (Alopecia Totalis), and even fewer people may progress to affect the hair on the whole body (Alopecia Universalis).
10 to 20 % of sufferers have tiny indentations on the surface of the nails (nail pittings), which are usually arranged in vertical or horizontal lines.
The diagnosis is easy and does not require any investigations. Tests may be done for the thyroid functions, particularly in children, as the chance of abnormalities is as high as 25%.
Progress
This is difficult to estimate. Most will recover on their own. In general, the younger the age of onset, and the larger the affected area, it is more unlikely to recover. For the very large sizes; hair outside the scalp; alopecia totalis, or alopecia universalis, the chance of recovery is much smaller.
In the first attack, most people will recover in 1 to 2 years : 30% in the first 6 months; and 50% in the first year. However, some people may never have the hair grown back, and for those who have recovered, 50% will have a new attack at a new place.
Treatments
Steroid
Small areas can be treated with injection of steroid. Usually there is new hair coming out 4 to 6 weeks after the injection, and it can be repeated after 1 month if necessary. It is more effective to use an injection gun designed to inject substances into the dermis by vacuum pressure. The pain is less and the accuracy of injecting into the dermis is higher.
 |
 |
 |
|
Before |
Immediately After |
1 month Later |
If there is no response after 3 months, then it may not be necessary to continue. It can be repeated again if the condition recurs. For those ones that have persisted for a long time without recovery, the chance of success is very low.
Minoxidil Lotion
It is applied twice daily on the affected area. Evidences of its effectiveness in the clinical studies are not consistent and vary a great deal. It is usually regarded as a supplementary treatment in addition to steroid injection.
Mesotherapy
The concept of mesotherapy is to inject directly a small quantity of some ingredients into the dermis of the skin, to exert a positive treatment result in and around that area. This method has been and is still very popular in Europe, in various branches of Medicine.
Mesotherapy is now used in treating cellulites, tightening lax skin, rejuvenating aging skin, treating scars and hair loss.
The doctor will mix a cocktail of different ingredients, including vitamin B5, vitamin H (Biotin), which are essential in hair growth and will increase the blood circulation in the scalp. In some cases, minoxidl can be added as well. It may have unexpected result in some resistant cases.
The depth of injection is only 3 to 4mm. The pain is tolerable. Usually a course of treatment consists of a weekly treatment for 3 to 4 weeks, and then a bi-weekly treatment for another 3 to 4 weeks.
Others
Treatments used in the past include phototherapy, and local irritants such as Dinitrochlorobenzene and Dithrano. The results were not encouranging.
Causes of Dandruff
Lots of people have experienced dandruff problems, which may be so heavy to look like snow flakes on their shoulders and causes a lot of embarrassment.
Sometimes the dandruffs may not be simple dandruffs, but are actually features of another skin disease such as psoriasis or seborrhoeic dermatitis, in which cases they are much thicker and bigger.
Where Does Dandruff Come From?
The cells at the bottom layer of the skin split and the new cells will migrate upwards to replace those that have aged, died, and shed off at the surface. Under normal circumstances, this process is done in a controlled manner; the dead skin shed off in the scalp is hardly noticeable.
When the process is out of control in some diseases, the cells at the bottom may divide rapidly, with large number of unhealthy cells moving up the layers. The skin is thickened and the dead skin at the surface will be shed off more rapidly. The faster the shedding, the more dandruff will appear and become very noticeable.
Causes of Dandruff
It is not quite understood how this normal shedding process is disordered. Different theories include hormonal imbalance, bacterial or fungal contamination, food, excessive oily secretion, environment, and stress. None of these is confirmed to be a factor.
Normal excessive dandruff is usually small, and there is no inflammation or itching in the scalp. However, those in seborrhoeic dermatitis and psoriasis are much bigger and more severe.
Seborrhoeic Dermatitis
It is due to the presence of a fungus called Pityrosporum ovale. Apart from the heavier dandruff, the scalp is oily and itchy. There is inflammation, affecting the scalp, the eyebrows, the sides of nose, the chest and the back.
For details, please go to Skin Problems > Common Skin Problems > Eczema / Dermatitis > Seborrhoeic Eczema.
Psoriasis
Psoriasis can affect any part of the body. It appears as thick red plaques on the skin, with shinny scales on the surface. When it affects the scalp, the thick and greasy dandruff may matt together as a large piece and stick tightly to the hair. It can be very difficult to wash off or treat.
The cause of psoriasis is not known, but about 2 % of the population has it, and family genetic has a major role in its happening.
For details, please go to Skin Problems > Common Skin Problems > Psoriasis
Management & Treatments
It depends on whether there is another cause. The way to apply the medication is important too, because it has to bring the active ingredients to the affected area, but has to be cosmetically acceptable as well.
Medicated Shampoo
It is the easiest to use. However, due to the short contact time, the effect is small and only suitable to the mildest cases.
Solution
The contact time is longer. It is usually a steroid solution, which is used to reduce inflammation, but it is not too effective in removing large scales of dandruff.
Lotion & Ointment
They are generally messy and more difficult to use, and also difficult to wash off after use. However, if shampoo or solution cannot remove the scales, then it may become necessary. It is left over in the scalp for overnight to dissolve the scales, and is washed off the next morning after combing the hair with a fine-toothed comb, usually with a tar-containing shampoo.
Main Ingredients
Anti-fungals
This is effective for reducing the number of Pityrosporum ovale, which is a fungus causing seborrhoeic dermatitis. These include Sulphur, Zinc pyrithion, Selenium sulphide and Ketoconazole.
Tar
It can be divided into Coal Tar and Pine Tar. It can reduce the cell division, reduce inflammation, and reduce the itchiness.
Salicylic acid
It can dissolve the dead keratinocytes, and clear the scales faster.
Steroid
It is only suitable for use in the case of seborrhoeic dermatitis and psoriasis.
Calcipotriol
It is used only for psoriasis.
Treatment Regimes
Mild Dandruff
Regular, more frequent shampooing is usually all that necessary. Sometimes using shampoo that contains anti-fungals may speed up the result. There is some evidence that taking vitamin B6 may help dandruff.
Seborrhoeic Dermatitis & Psoriasis
Mild
Medicated shampoo is usually enough to control the situation. Selenium Sulphide, Ketoconazole and Pyrithion Zinc shampoos can target dandruff caused by seborrhoeic dermatitis. Tar shampoos can help both seborrhoeic dermatitis and psoriasis.
Moderate
Usually steroid is need. If there are more scales, the steroid can be combined with salicylic acid. Calcipotriol may be considered in psoriasis.
Severe
Apart from continue the use of steroid solution to reduce the inflammation; these resistant scales can be removed by applying an ointment containing sulphur and salicylic acid, which will dissolve the scales after being left in the scalp overnight. The ointment is avoided to mess up the beddings with a shower cap, and it is washed off the next morning with a tar shampoo.
Tinea Capitis
Similar to tinea coporis, tinea capitis is due to fungal infection of the skin, but it is only common in children before puberty. It is usually transferred from one child to another at school, except in the cases where the source is from animals, for example adult can contract tinea capitis from cows through contact.
Signs
One or more areas have some scattered hair loss and skin peeling off. There is usually inflammation with redness, of varying degree, but some may have none at all. Although it may occasionally cause itchiness, most people do not have any feeling, and it is usually discovered by the parents.
Generally speaking, fungus of animal origin causes more inflammation in tinea capitis. Sometimes it may be severe with large area of inflammation, folliculitis, boils, and pus formation.
Clinical Diagnosis
It is usually unnecessary to do any test for the diagnosis, but if the diagnosis is uncertain, a sample of skin scrapping or hair cut from the area can be sent for laboratory testing.
An ultra violet light (Wood’s light) can help in the diagnosis, where some (not all) fungal infections of the scalp will turn a fluorescent green or yellow under this light.
If it is a case of animal fungus type infection, then it may be necessary to examine those animals that have been in contact, such as the pets at home.
Treatments
School children suffering from tinea capitis have to stay away from attending school, usually after having used the medicated shampoo and oral treatment for 5 days. Fellow schoolmates need to be examined for the signs of tinea capitis, while close contact such as family members need to use medicated shampoo to reduce the chance of carriage.
The fungal spores can exist in the inside or outside of the hair shaft. Usually it is the external one that is more difficult to treat and will require a longer course of treatment.
Medicated Shampoo
It usually contains ketaconazole. However this external treatment is not totally effective when used on its own, because it cannot penetrate deep enough into the centre of hair follicles and the hair root. It should be regarded only as a supplementary treatment, to reduce the number of fungal spores on the outside of hair shaft and therefore the spread, as well as to speed up the recovery.
Oral Treatments
In the past, the traditional treatment has been Griseofulvin, which has a very good safety profile in children. The usual course is 4 to 6 weeks of treatment, with some types of fungi needing a longer course. The incidence of fungi becoming resistant to griseofulvin has increased a lot recently.
Terbinafine and Itraconazole have been shown more recently to be safe too in children, and because of their much better efficacy, more and more doctors have turned to prescribe them instead.
The course of Terbinafine is 2 to 4 weeks. The cure rate can be as high as 80 to 100%. Some types of fungi may require a longer course. For those cases of external spores, the cure rate is not too satisfactory, even when the course is increased to 8 to 12 weeks.
Itraconazole has the same course period of 2 to 4 weeks, and again may require a longer period for some types of fungi. The cure rate is similar to Terbinafine. It has a suspension preparation, which is more convenient for small children. It can also be taken in a cyclical regime, where only 1 week’s treatment is taken in a given month. The cure rate can be as high as 90% after 2 to 3 cycles.