This is caused by the Varicella Zoster Virus (VZV). It appears as chicken pox when the person is first infected with it. Chicken pox is a very common childhood infection, and almost every one of us has been infected. Although we are immune from repeated infection after the resolution of chickenpox, VZV lies dormant in the nervous system in the spinal cord.
The VZV is usually under inhibition by our immune system. When the immunity is low, it will be reactivated, travels from the spinal cord to the skin surface via 1 or 2 particular nerves, and results in rash with blisters. This is herpes zoster.
A person of any age with a prior chicken pox may develop zoster, but incidence increases with advancing age due to declining immunity. Any factors that may lower the immune activity may also cause the reactivation, such as over tiredness, time of a cold or other illnesses, taking some medications such as steroid or other immuno-suppressants.
Signs & Symptoms
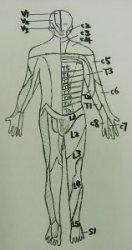
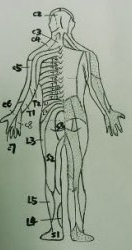
Our nerves are divided into either left or right side, and each nerve supplies an area we call a dermatome. Therefore the viruses will travel through the nerves to the related dermatomes on one side only.
|
|
|
The most commonly affected areas are the chest (T4, T5), the waist (T10, T11), and the upper face (V1). However, it can happen in any areas, but is generally limited to 1 dermatome or at most 2 or 3 adjacent dermatomes in normal hosts.
|
|
|
While the viruses are traveling in the nerves before reaching the skin, the inflammation of the nerve (neuritis) will result in some altered sensations in the related dermatomes. These include itch, tingling, ache and pain. It can be mistaken as a muscle sprain in the waist, or in some cases even a heart attack when it happens on the chest.
Then in the next few days, a rash appears, initially like urticaria, but very quickly painful blisters develop in the rash. Most patients describe the pain as burning, throbbing, or stabbing. The blisters slowly dry up and crust over 7 - 10 days. The whole recovery takes up to 2 - 3 weeks.
Diagnosis
It is based primarily on the history of prodromal pain, and the characteristic location and appearance of the skin eruption. In some patients, the presentation can be atypical and may require additional testing such as smear and DNA tests.
Complications
It usually has a benign course, but complications may occur. There may be superimposed infection from other bacteria, as the host’s immunity is already lowered.
The pain in the dermatome may continue even when the rash has apparently resolved. This is called post-herpetic neuralgia, and is more common in patients more than 50 years old. The pain usually resolves within 6 months, but more than 1% of patients continue to have pain for a long time, and it can be excruciating.
When it affects the upper face, it may be associated with inflammation of the cornea, which may ulcerate and lead to blindness.

Less common complications are involvement of cranial nerves and the brain, which can be very delibitating.
Managements & Treatments
Although herpes zoster usually resolves in 2 to 3 weeks, but it is important to shorten the duration for pain, as well as to reduce the chance of complications.
The usual treatment is with high doses of acyclovir, 800mg taken 5 times per day, for 1 to 2 weeks. The newer generations, valacyclovir and famciclovir, have better bio-availability, can be taken only 2 - 3 times per day, and apparently are more effective. For those people with widespread disease because of poor immunity, treatment with intravenous acyclovir may be required.
The pain can be managed by simple paracetamol, but stronger analgesics would be need for more severe pain. If there is co-existing bacterial infection, topical or oral antibiotics are needed.
It the herpes zoster involves the area on the nose tip, or around the eye, the cornea may be affected and it requires the examination by an opthalmologist.The addition of oral steroid has no effect on the development or duration of post-herpetic neuralgia. Carbamazepine and amitriptyline are sometimes used to treat post-herpetic neuralgia. Severe cases may require the help of an anaethetist, who will need to cut the nerve involved to relieve pain.
As the current medications cannot penetrate into the nervous system and kill all the viruses, herpes zoster may happen again in subsequent years, but may in a different area.